Peptic ulcers are open sores that develop on the lining of the stomach, upper small intestine, or esophagus. While most peptic ulcers can be treated with medications and lifestyle modifications, surgery may be necessary in certain cases. In this article, we will explore the reasons for peptic ulcer surgery, the types of surgical procedures involved, the recovery process, and the potential risks and complications associated with the surgery.
Understanding Peptic Ulcers
Peptic ulcers are typically caused by an imbalance between the stomach’s protective mechanisms and the presence of harmful factors such as Helicobacter pylori (H. pylori) infection, prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs), excessive alcohol consumption, or smoking. These ulcers can lead to symptoms such as abdominal pain, bloating, heartburn, and nausea.
When is Peptic Ulcer Surgery Necessary?
Peptic ulcer surgery is considered when the ulcers do not respond to conservative treatment measures or when complications arise. Common indications for surgery include:
- Bleeding ulcers: When an ulcer causes significant bleeding that cannot be controlled with medications or endoscopic procedures.
- Perforation: If an ulcer forms a hole in the stomach or intestine, requiring immediate surgical repair.
- Obstruction: When the ulcer causes a blockage in the digestive tract, leading to severe symptoms and impaired passage of food.
Preparing for Peptic Ulcer Surgery
Before undergoing peptic ulcer surgery, proper preparation is necessary. This typically involves:
- Medical evaluations: Assessing overall health and conducting necessary tests to ensure readiness for surgery.
- Medication adjustments: Adjusting or discontinuing certain medications, such as blood thinners, that may interfere with the surgical procedure.
- NPO status: Following fasting guidelines, typically starting the night before the surgery.
Types of Peptic Ulcer Surgery
There are different types of surgical procedures for peptic ulcers, depending on the specific condition and individual factors. The common surgical interventions include:
- Vagotomy: Involves cutting or sealing the vagus nerve to reduce acid production in the stomach.
- Antrectomy: The removal of the lower portion of the stomach (antrum) where most acid production occurs.
- Gastrectomy: Removal of a portion of the stomach, often performed in more severe cases or when malignancy is suspected.
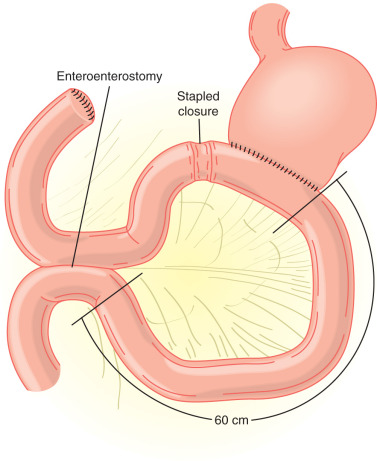
- Bypass procedures: Involves rerouting the digestive tract to bypass the ulcerated area.
The Surgical Procedure
The specific surgical procedure chosen will depend on the individual’s condition and the surgeon’s recommendation. The surgery is typically performed under general anesthesia and may involve laparoscopic (minimally invasive) or open approaches. During the procedure, the surgeon will address the underlying issue, such as repairing perforations, removing the ulcerated tissue, or modifying the stomach to reduce acid production.
Recovery and Post-operative Care
Recovery from peptic ulcer surgery can vary depending on the type and extent of the procedure. Following surgery, patients will be monitored in the hospital for a certain period. Pain management, wound care, and diet modifications will be part of the post-operative care plan. The healthcare team will provide instructions on medication usage, dietary restrictions, and follow-up appointments.
Risks and Complications
As with any surgical procedure, peptic ulcer surgery carries some risks and potential complications. These may include infection, bleeding, anesthesia-related complications, leakage at the surgical site, or post-operative bowel dysfunction. It is important to discuss these potential risks with the surgeon beforehand.
Long-term Outlook
Peptic ulcer surgery can provide relief from symptoms and prevent complications in cases where conservative treatment options have failed. The long-term outlook depends on various factors, including the underlying condition, the success of the surgical intervention, and adherence to post-operative instructions. It is essential to maintain a healthy lifestyle, including dietary modifications and medication management, to prevent the recurrence of ulcers and promote overall well-being.
Frequently Asked Questions
- Will I be awake during peptic ulcer surgery?
- No, peptic ulcer surgery is typically performed under general anesthesia, which means you will be unconscious and unaware during the procedure.
- How long does it take to recover from peptic ulcer surgery?
- The recovery time can vary depending on the type of surgery performed and individual factors. It may take several weeks to months to fully recover and resume normal activities.
- Will I still need to take medications after peptic ulcer surgery?
- The need for continued medication usage after surgery will be determined by your healthcare provider. In some cases, medications to manage stomach acid production or prevent H. pylori infection may still be required.
- Can peptic ulcers recur after surgery?
- While surgery can effectively treat peptic ulcers, there is a small possibility of recurrence. Adhering to post-operative care instructions, making necessary lifestyle modifications, and regularly following up with healthcare providers can help minimize the risk of recurrence.
- Will I need to make dietary changes after peptic ulcer surgery?
- Dietary changes may be necessary after peptic ulcer surgery to support healing and prevent complications. Your healthcare team will provide specific guidelines regarding your diet, including any restrictions or modifications needed.
Conclusion
Peptic ulcer surgery becomes necessary when conservative treatment options fail or when complications arise. Understanding the indications for surgery, the types of procedures involved, the recovery process, and potential risks and complications is important for individuals considering or undergoing peptic ulcer surgery. With proper preparation, post-operative care, and adherence to healthcare providers’ instructions, individuals can improve their long-term outlook and enjoy relief from symptoms associated with peptic ulcers. Remember to consult with healthcare professionals for personalized advice and to address any concerns specific to your situation.

